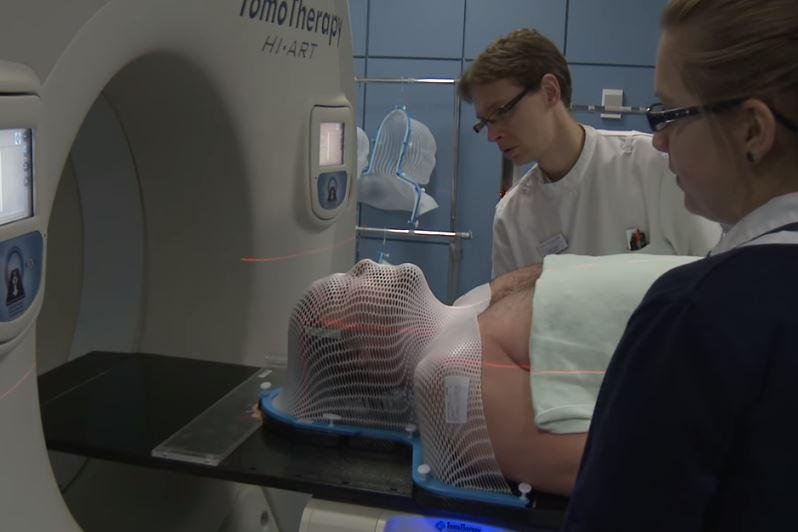
A clinical trial found patients' cognitive functions can be preserved if the hippocampus portion of the brain is avoided during radiation. Screenshot courtesy of Cancer Research UK
Oct. 23 (UPI) -- Patients' cognitive functions can be preserved if the hippocampus portion of the brain is avoided during radiation, according to the results of a clinical trial.
Researchers compared hippocampal-avoidance radiotherapy with traditional whole-brain radiation for patients with brain metastases. They presented their practice-changing findings Tuesday at the American Society for Radiation Oncology Annual Meeting in San Antonio and are in the process having them published in an academic journal.
The hippocampus, which is located under the cerebral cortex, is the part of the brain associated with cognitive function, including memory.
In brain metastases, cancer cells have spread to the brain from primary tumors in other organs.
Brain metastases affect up to 45 percent of adults with cancer and they account for 20 percent of cancer deaths annually.
Whole brain radiotherapy currently is the most effective treatment for brain metastases, but it often is the last resort because of cognitive decline.
"Using this approach, patients can benefit through optimal control of brain metastases, prevention of new brain metastases and better preservation of their cognitive function and quality of life," lead author Dr. Vinai Gondi, director of research at the Northwestern Medicine Chicago Proton Center, told UPI.
Researchers used intensity-modulated radiation to shape the radiation beams to avoid central regions within the brain while treating the rest of it with therapeutic doses of brain irradiation.
Proton therapy also utilizes a precise dose of radiation that conforms to the shape of the tumor. This reduces the risk of side effects and damage to surrounding healthy tissues.
"Sparing these neural stem cells of significant doses of radiation during brain irradiation prevents damage to these important neural stem cells and this preserves cognitive function," Gondi said.
The trial was conducted throughout the United States and Canada as well as some locations in other countries.
In the study, 518 patients with a median age of 61.5 years randomly received whole brain radiotherapy plus memantine with or without hippocampal avoidance from 2016 to last March. They found a 26 percent relative reduction in risk of cognitive toxicity with hippocampal avoidance compared with whole brain radiotherapy. The cognitive function benefit didn't differ by age.
Favorable follow-up results were at four, six and 12 months.
"This hippocampal-sparing approach reduces both the risk of growth of new brain metastases and the risk of cognitive decline, and no prior study has ever demonstrated this dual effect," Dr. Walter J. Curran, executive director of the Winship Cancer Institute at Emory University, said in a press release.
Gondi said any patient who presents with brain metastases should be considered for the procedure if their expected survival is anticipated to be four months or longer.
"Brain metastasis patients can currently receive this treatment approach," Gondi said. "In fact, as part of this and preceding/concurrent trials, our research team trained and credentialed several hundred physicians across community, academic and international centers in our techniques for hippocampal sparing."
The Northwestern Medicine Chicago Proton Center is the first and only proton therapy center in Illinois, and is one of 28 in the United States.
This new research builds upon decades of preclinical and clinical research on the importance of the hippocampus on brain irradiation, researchers said.
"The results of this trial could have a significant impact on patients," Dr. Paul Brown, a radiation oncologist at Mayo Clinic and co-author on the new study, said in a press release.