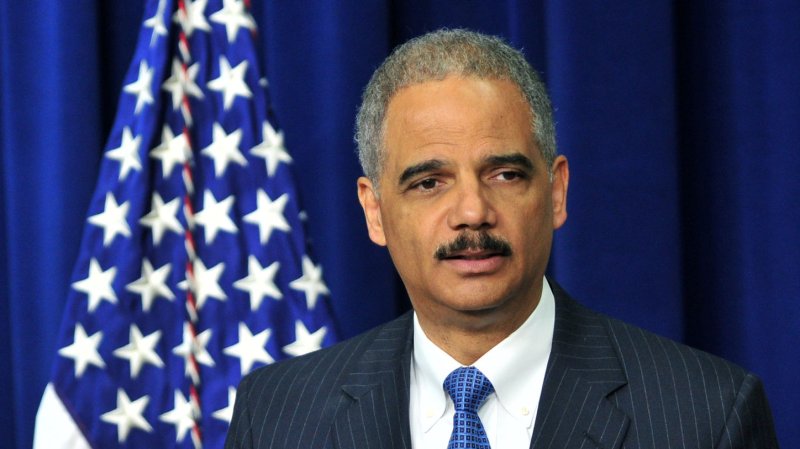
U.S. Attorney General Eric Holder said Medicare fraud schemes involved about $452 million in false billing. UPI/Kevin Dietsch |
License Photo
WASHINGTON, May 2 (UPI) -- A nationwide operation against Medicare fraud has resulted in charges against 107 suspects, including doctors and nurses, U.S. officials said Wednesday.
U.S. Attorney General Eric Holder and other officials said the Medicare fraud schemes involved about $452 million in false billing in seven cities.
The coordinated operation involved the highest number of false Medicare billings in a single sweep in the history of the Medicare Fraud Strike Force.
Department of Health and Human Services also suspended or took administrative action against 52 healthcare providers following a data-driven analysis and credible allegations of fraud. Officials said the new healthcare law, the Affordable Care Act, significantly increased HHS' ability to suspend payments until an investigation is complete.
Court documents said the defendants allegedly participated in schemes to submit claims to Medicare for treatments that were medically unnecessary and often never provided. In many cases, court documents allege, patient recruiters, Medicare beneficiaries and other co-conspirators were paid cash kickbacks in return for supplying beneficiary information to providers, so that the providers could submit fraudulent billing to Medicare.
"The results we are announcing today are at the heart of an administration-wide commitment to protecting American taxpayers from healthcare fraud, which can drive up costs and threaten the strength and integrity of our healthcare system," Holder said.
Those charged included 59 defendants in Miami; 22 in Detroit; nine in Houston and seven in Baton Rouge, La., among other cities.