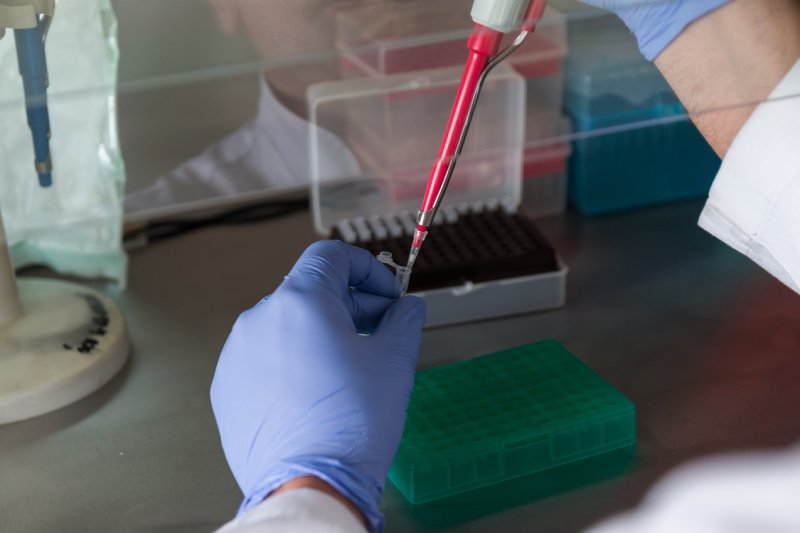
Liquid biopsy may be useful in prediction of breast cancer recurrence. Photo by
jarmoluk/Pixabay
Dec. 13 (UPI) -- A new tool could make it easier to predict whether early-stage triple-negative breast cancer will return following chemotherapy.
In study results expected for presentation Friday at the 2019 San Antonio Breast Cancer Symposium, researchers used a liquid biopsy -- FoundationOne Liquid, manufactured by a company called Foundation Medicine -- that detects circulating tumor DNA, or ctDNA, in a blood test to predict cancer recurrence.
"If you are a woman with triple-negative breast cancer, after surgery you are in a constant 'watch and wait' scenario, in fear of the cancer coming back," said study co-author Milan Radovich, an associate professor of surgery and medical and molecular genetics at Indiana University School of Medicine. "We know that a significant proportion of these women will have disease relapse after surgery. ctDNA is a powerful tool to be able to predict recurrence and could help us identify the best ways to manage care for women diagnosed with this disease."
For the study, the researchers analyzed blood plasma samples collected from 196 women enrolled in the BRE12-158 clinical trial, led by researchers at Indiana University. They sequenced ctDNA -- breast cancer tumor DNA visible in blood plasma -- in 142 of the women using the FoundationOne Liquid Test.
Overall, they were able to detect mutated ctDNA in 90, or 63 percent, of the women, with TP53 being the most commonly mutated gene. TP53 mutations have been associated with breast cancer.
After following study participants for nearly 18 months, the authors found that detection of ctDNA was "significantly associated" with poorer distant disease-free survival, or DDFS. Women with ctDNA in their blood plasma had a median DDFS of 32.5 months and, at 24 months, the probability of DDFS was 56 percent in women who were positive for ctDNA and 81 percent in those who were ctDNA-negative.
After accounting for tumor size, grade and, stage as well as the age and race of the participants, they found that ctDNA-positive women were three times as likely to have distant disease recurrence than those who were ctDNA-negative. In addition, ctDNA-positive women were found to have a risk for death 4.1 times higher than ctDNA-negative women.
"In the curative setting, telling a patient they are at high risk for recurrence isn't overly helpful unless you can act on it," senior author Bryan P. Schneider, a professor of medicine and medical and molecular genetics at Indiana University School of Medicine, told UPI. "What's more important is the ability to act on that in a way to improve outcome."
Historically, comprehensive genomic profiling has been used to identify predictive biomarkers for disease or disease recurrence and match patients with targeted therapies, immunotherapies and possible clinical trials.
In general, additional research is needed to determine if the use of liquid biopsy to detect ctDNA can be incorporated into clinical practice to predict disease recurrence in breast cancer, as well as other solid-tumor cancers.
Based on these and other study findings, ctDNA is being explored as a way to detect cancer, guide treatment and monitor patients during remission. In addition, the authors of the Indiana University study said they plan to start a clinical trial next year that will further examine ctDNA's potential in guiding therapy for those patients who are at high risk of breast cancer recurrence.
Brian Alexander, chief medical officer at Foundation Medicine, told UPI the liquid biopsy is being used in patients with advanced cancer "for whom tissue biopsy may not be feasible." The approach is also used in comprehensive genomic profiling, or CGP, which can identify genetic alterations found in certain types of cancer and help guide targeted therapy approaches for these tumors.
Alexander said company figures suggest only 15 percent of patients with advanced cancer are receiving CGP, and more than 60 percent of cancer patients aren't receiving any form of genomic testing.
"We believe all advanced cancer patients should receive comprehensive genomic profiling at diagnosis to help inform treatment planning," he said. "As more options for personalized cancer care become available, comprehensive genomic profiling could have the greatest clinical benefit when used to guide therapy decisions early in the treatment process by uncovering and guiding patients to their potential treatment options."