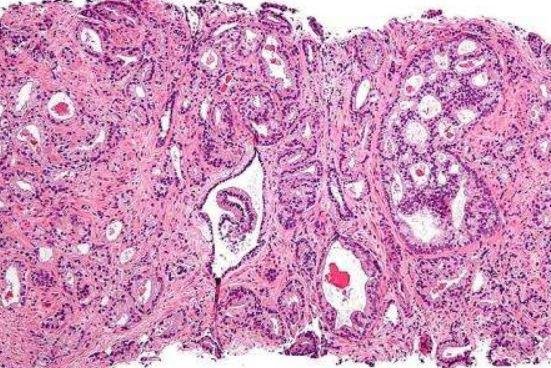
This micrograph shows the most common form of prostate cancer: prostatic acinar adenocarcinoma. A study found immunotherapy may effectively treat men with the aggressive prostate cancer. Photo by
Nephron/Wikimedia Commons
Sept. 5 (UPI) -- Researchers have found immunotherapy may effectively treat men with aggressive prostate cancer, raising the possibility of new treatments.
Men with aggressive prostate cancer are good candidates for immunotherapy because the unstable tumors are more likely to stimulate an immune response than other cancers, according to researchers at The Institute of Cancer Research in London and the Dana-Farber Cancer Institute in the United States. Their findings were published Tuesday in the Journal of Clinical Investigation.
For aggressive prostate cancer, the 10-year survival rate for men is 26 percent, according to The Prostate Center in England.
Immunotherapy includes manmade versions of immune system proteins, drugs that basically take the "brakes" off the immune system, cancer vaccine and treatments that boost the immune system in a general way, according to the American Cancer Society.
The scientists studied why some men with advanced prostate cancer have much worse survival than others.
"Our study found that some men with advanced prostate cancers have genomic mutations in their tumors that make the disease unstable, aggressive and resistant to standard therapies," study leader Dr. Johann de Bono, a professor of cancer research at The Institute of Cancer Research, said in a press release. "These men with 'mismatch' repair mutations only live about half as long as others who also have advanced prostate cancer but whose tumors don't carry such mutations."
Based on their study results, researchers with the Institute of Cancer Research and The Royal Marsden are testing the effectiveness of checkpoint inhibitor immunotherapies in clinical trials.
Researchers previously looked at 127 tumor biopsies from 124 patients and genomic information from 254 patients acquired by the Prostate Cancer Foundation/Stand Up to Cancer International Prostate Cancer Dream Team.
They found that 8.1 percent of men with advanced prostate cancer had evidence of mismatch repair mutations in their tumors. They survived only 3.8 years after beginning prostate cancer treatment compared with 7.0 years for men with no detectable mismatch repair defects.
"Mismatch repair" gene mutations in cancers can't correct single-letter mistakes in their DNA code properly and are genetically unstable. As they grow and rapidly evolve drug resistance they acquire more mutations.
The researchers thought these cancer cells might be particularly easy for the immune system to recognize because they look different from healthy cells.
In searching for a likely response, they examined levels of a protein called PD-L1 on the surface of cancer cells. By targeting PDL-1 activity with an immune checkpoint inhibitor, the immune system was free to attack cancer cells.
Half of tumors with mismatch repair mutations had high levels of PD-L1 compared with only 9.8 percent without these mutations. In addition, more than half of the tumors with mismatch repair mutations were invaded by T cells from the patient's immune system.
"Immunotherapy is an unusual treatment in working best in cancers that have a lot of mutations," said Paul Workman, chief executive of The Institute of Cancer Research Prostate. "Prostate cancers normally tend to have fewer mutations than other cancer types, which may be why immunotherapy has so far only been successful in a small minority of patients.
"It will be fascinating to see whether we can translate the theory into practice in the new clinical trials to test out immunotherapy in men with genetically unstable tumors."