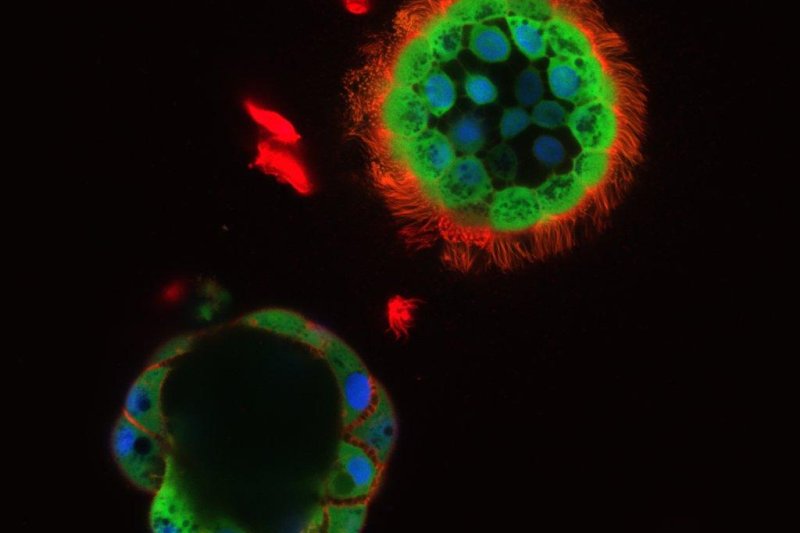
A microscope image shows a pair of nasospheroids being exposed to cystic fibrosis drugs. Photo by UNC
Nov. 21 (UPI) -- Scientists have developed a new test to determine which cystic fibrosis treatment is best suited to an individual patient. The new test is part of a broader effort to personalize medicine.
Several new drugs have improved health outcomes for patients with cystic fibrosis, a genetic disorder that affects the lungs. Despite improvements, not every drug works for every patient.
Trial and error is cost prohibitive, as many of the drugs are several thousand dollars and take months to take effect. Some can cause adverse side effects. It's imperative doctors prescribe the proper drug, or combination of drugs, the first time.
While cystic fibrosis is caused by the absence of a properly functioning CFTR gene, more than 2,000 genetic mutations are associated with a malfunctioning CFTR gene. Different combinations of mutations can affect the severity of the disorder, as well as the effectiveness of different treatments.
"Any given drug may not be the drug that works best for a given patient, because there's so much variation from person to person," Dr. Jennifer Guimbellot, who conducted the latest research while working at the University of North Carolina, said in a news release.
Currently, the best test to determine whether or not a drug will be effective involves a rectal biopsy, followed by complex manipulation of biological samples in the lab. But Guimbellot and her colleagues have developed a less invasive method to determine which drugs work best.
Cystic fibrosis causes sticky mucus to build up in the lungs, making patients' prone to infections. A lack of hydration throughout the respiratory system prevents proper drainage.
While working with Dr. Martina Gentzsch, an associate professor of cell biology and physiology at UNC, Guimbellot noticed little fluid-filled balls called nasospheroids inside the nasal cavities of cystic fibrosis patients. The researcher realized they could extract cells from the nasal cavity of patients and allow nasospheroids to form. The fluid-filled balls can then be used to test the effectiveness of different CFTR drugs.
"When CFTR is turned on, the balls shrink down -- mediated by the transport of salt and water -- and we can quantify that by measuring the size of the balls," said Guimbellot, now a professor of pediatrics at the University of Alabama at Birmingham.
The test is simple and less invasive, and the early results -- published this week in the Journal of Clinical Investigation Insight -- suggest it is also accurate.
"We still have a long way to go to get a really optimized therapy for most cystic fibrosis patients, and the only way we can do that is to have a model like ours, where we can take cells from each individual patient and test them with each individual drug to find out which one is the best match," Guimbellot said.