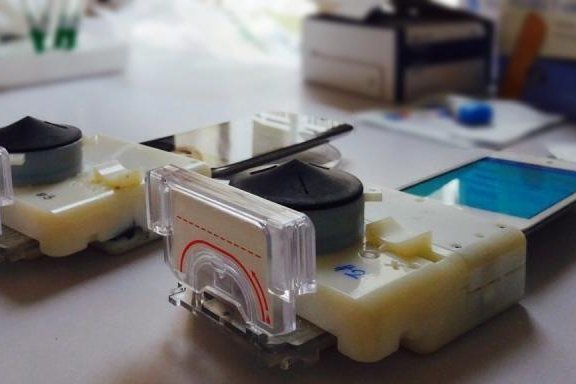
The dongles can detect HIV and syphilis in under 15 minutes. Photo by Samiksha Nayak/Columbia Engineering.
NEW YORK, Feb. 5 (UPI) -- Need to get tested for STDs? There's app for that -- sort of.
A new, low-cost smartphone accessory allows healthcare professionals to return HIV and syphilis diagnoses in less than 15 minutes, and it could be programmed to detect other sexually transmitted diseases.
The device, which attaches to a smartphone, uses a pinprick to collect a small blood sample. The sample is analyzed for three biomarkers using a process called an enzyme-linked immunosorbent assay.
All the moving parts (mechanical, optical, and electronic) of the testing process -- typically performed in a lab -- are condensed and confined to the device. The smartphone is only used as a power source.
"Our work shows that a full laboratory-quality immunoassay can be run on a smartphone accessory," Samuel K. Sia, an associate professor of biomedical engineering at Columbia Engineering, explained in a press release.
"Coupling microfluidics with recent advances in consumer electronics can make certain lab-based diagnostics accessible to almost any population with access to smartphones," said Sia, who helped lead the efforts to develop the device. "This kind of capability can transform how health care services are delivered around the world."
Whereas most comparable equipment costs upwards of $20,000, the new dongles, (an accessory that can be plugged into a phone or computer), can be manufactured for $34. The low cost and minimal energy usage will make it ideal for health care providers in many parts of Africa, where HIV remains prevalent but access to medical equipment and electricity can be spotty. Sia and his colleagues successfully tested the device on nearly 100 patients in HIV clinics in Rwanda
"We are really excited about the next steps in bringing this product to the market in developing countries," Sia concluded. "And we are equally excited about exploring how this technology can benefit patients and consumers back home."
The device is detailed in the newest issue of the journal Science Translational Medicine.